Fiber is one of the most talked-about nutrients in nutrition — and one of the most misunderstood.
If you’ve ever felt bloated, constipated, constantly hungry, or stuck on a blood sugar rollercoaster… fiber may be part of the missing piece.
But here’s the relief:
You don’t need to overhaul your entire diet.
You don’t need extreme changes.
You don’t need perfection.
You need clarity.
Let’s simplify it.
How Much Fiber Should You Eat Per Day?
According to established recommendations:
Women (ages 19–50): 25 grams per day
Women (over 50): 21 grams per day
Men (ages 19–50): 38 grams per day
Men (over 50): 30 grams per day
These targets give your digestive system, blood sugar regulation, cholesterol levels, and fullness signals the support they need.
Most adults, however, are falling short.
And that gap often shows up as symptoms.
What Happens When Fiber Intake Is Too Low?
Low fiber intake can contribute to:
Sluggish digestion or constipation
Energy dips
Increased cravings
Blood sugar spikes and crashes
Feeling hungry shortly after eating
At Compass Nutrition, we don’t chase restriction.
We focus on relief — and often, relief begins by adding support rather than removing food.
Fiber is one of those quiet, powerful supports.
High-Fiber Foods That Make It Easy
The goal isn’t to memorize numbers. It’s to recognize patterns.
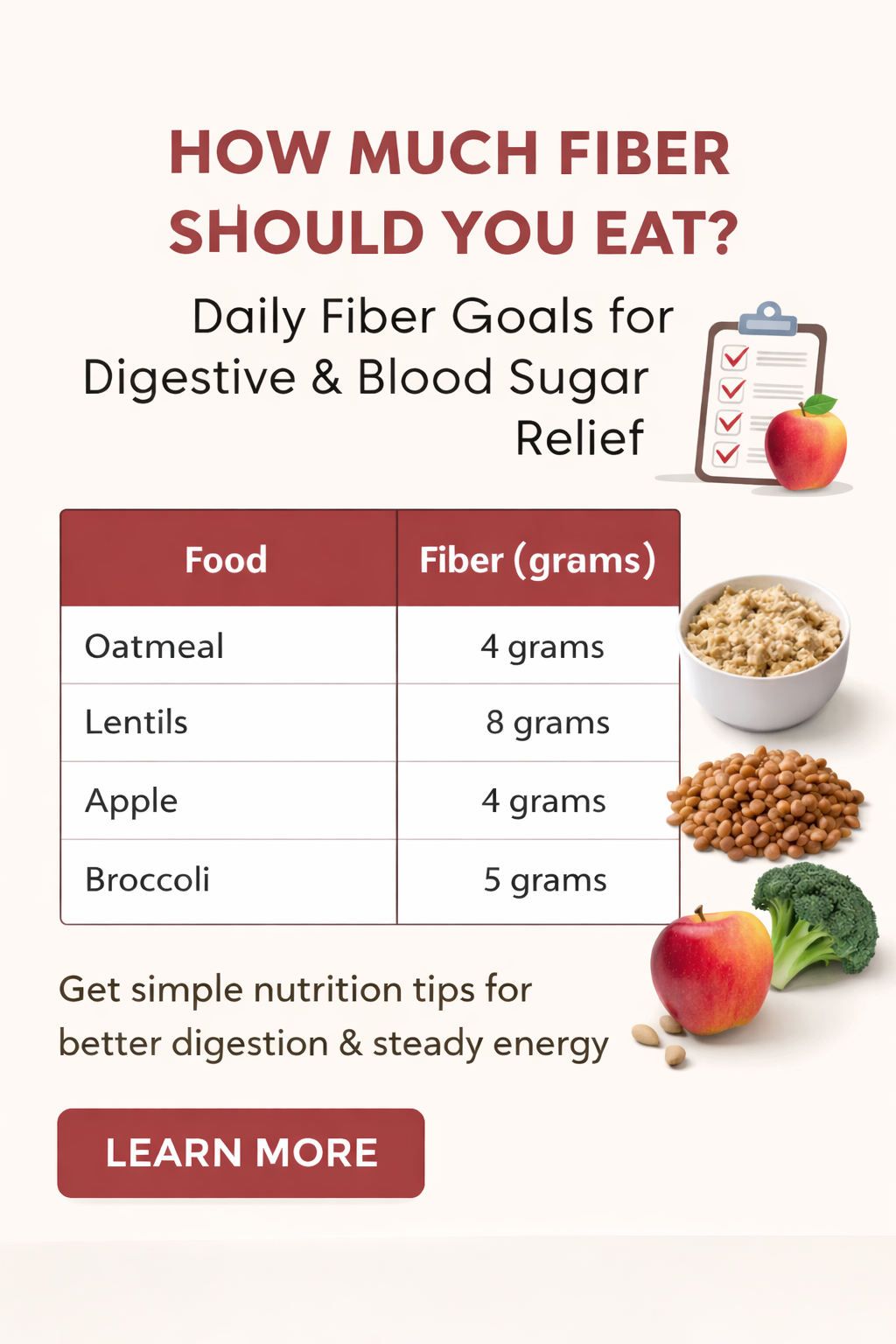
Here are simple, everyday foods and their fiber content (from your downloadable guide):
Oatmeal (1 cup cooked): 4g
Apple with skin (1 medium): 4g
Lentils (½ cup cooked): 8g
Broccoli (1 cup cooked): 5g
Whole-wheat bread (1 slice): 2g
Almonds (1 ounce / ~23 nuts): 3.5g
Brown rice (1 cup): 3.5g
Carrots (1 cup raw): 3.5g
Raspberries (1 cup): 8g
Chia seeds (1 tablespoon): 5g
A breakfast of oatmeal + raspberries + almonds?
You’re already over 10 grams before lunch.
That’s how we build momentum — gently and realistically.
A Relief Approach to Increasing Fiber
If you’ve ever increased fiber too quickly and felt worse (gas, bloating, discomfort), you’re not alone.
Here’s the Compass Nutrition way:
1. Increase gradually
Add 3–5 grams per day at a time.
2. Pair with hydration
Fiber works best when fluids support it.
3. Distribute it across meals
Instead of cramming fiber into one meal, spread it out.
4. Focus on food first
Whole foods provide fiber plus vitamins, minerals, and phytonutrients.
Relief is rarely found in extremes.
It’s found in steady support.
Fiber & Blood Sugar: A Quiet Power Tool
Fiber slows digestion.
That means steadier glucose levels.
That means fewer crashes.
That means fewer cravings.
For patients on GLP-1 medications, individuals managing prediabetes, or anyone dealing with afternoon energy dips, fiber becomes foundational.
Not flashy.
But powerful.
When Fiber Needs Personalization
Not everyone benefits from high fiber in the same way.
Some individuals with:
IBS
Chronic bloating
Food sensitivities
Post-infection gut changes
GLP-1 medication side effects
…may need tailored adjustments.
That’s where individualized nutrition care matters.
Because relief isn’t one-size-fits-all.
Ready for More Digestive Relief?
If you’re unsure whether you’re hitting your fiber targets — or if symptoms are lingering despite “eating healthy” — let’s take a closer look.
Schedule a Nutrition Appointment
We’ll assess intake, symptoms, labs, medications, and lifestyle patterns to build a plan that supports your digestion and overall metabolic health.
Personalized 1:1 nutrition support
Final Takeaway
Fiber isn’t about chasing a number.
It’s about creating stability.
Steadier digestion.
Steadier blood sugar.
Steadier hunger signals.
And that steady feeling?
That’s where relief begins.